UTAR Centre for Research on Communicable Diseases (CRCD), in collaboration with Department of Soft Skills Competency (DSSC) of Sungai Long Campus, organised a physical and virtual talk titled “Hepatitis C: The Journey from Discovery to a Cure” on 15 September 2020. The event saw the attendance of about 140 participants.

Dr Chung delivering his talk
Invited to deliver the talk was Dr
Chung Yun Chien, a Consultant Hepatologist and Gastroenterologist at
Hospital Selayang. In his
talk, Dr Chung
first provided
a general idea on Hepatitis C (HCV).
“Hepatitis C Virus
is essentially an RNA virus.
There are five main types of hepatitis viruses, namely A, B, C, D and E. All
the hepatitis diseases are RNA viruses except Hepatitis B, which is a DNA
virus. There are other types of RNA virus of
Flavivirus
such as Dengue,
Yellow Fever
and Zika
Virus.
No vaccine is currently available
to prevent
Hepatitis
C,
but there
is a vaccine for Hepatitis B.
It is actually similar to the dengue virus. To date, there is no vaccine to
prevent the complication and development of dengue virus,” he said. He added
that the issue with the Hepatitis C virus is the heterogeneity of the virus
itself, which allows the virus to escape from the host immune system and
medications as well as vaccines.
He presented
the worldwide
distribution of
HCV
genotypes, saying that
HCV genotype three (54.5
per cent) was the most
prevalent genotype in Malaysia,
followed by genotype one (40
per cent).
He also explained what would happen if an individual was exposed to HCV and
he pointed out its
difference with Hepatitis B (HBV). “Between 2003 and 2017, only about 23,000
Hepatitis C had been notified to the MOH. This is just the tip of the
iceberg. There are a lot of people walking around with Hepatitis C without
knowing it. It was reported
that the incidence of Hepatitis C had increased from 2.65 per 100,000
populations in 2015. Regardless of
males or females, slightly
more than
50 per cent
of the patients were in the younger
age group
that is between 26 and 45
years old. Most of the reported patients were of
Malay ethnicity,”
said Dr Chung. He stressed
that the figure presented was dependent on
how the case was reported.
He also
demonstrated the projection of the current and future disease burden of HCV
infection in Malaysia and explained the exposure known to be associated with
HCV infection such as injecting drug use and sharing needles, blood
transfusions before the year 1994 (transplanted from an infected donor),
occupational exposure to blood, birth to an HCV-infected mother, and sex
with an infected partner. Furthermore, he explained how to determine an
individual who has been infected with the HCV virus and who
should be screened for HCV.
“Hepatitis C can be cured. Treatment should be given to every individual
regardless of who they are, where they come from, and the status of their
liver disease,” he said.
Dr Chung moved on to a more
positive note, in which he spoke about the treatment of HCV, which was the
most important part of the talk. He stated that the primary goal of therapy
would be to cure HCV for everyone infected. “Those cured of HCV would have
their blood show a sustained virologic response (SVG), after 12 weeks of
treatment. The cured patients tend to have reduced liver inflammation,
improvements in extrahepatic manifestation and liver necroinflammation,
regression of hepatic fibrosis and reduced risk of liver cancer, or
Hepatocellular Carcinoma (HCC),” said Dr Chung. He also reminded the
participants that while everyone with HCV should be treated, there are three
categories of people that need to receive prioritised treatment to prevent
the spread of the disease. Speaking on this, he added, “There are the
highest priority patients, which consist of those in need of an organ
transplant, who have advanced fibrosis (F3 to F4) and extra-hepatic
manifestations. Then comes the high priority patients, which are patients
with fibrosis 2 or more, co-infected with Hepatitis B (HBV) or HIV or with
other chronic lung diseases (CLD). Lastly, there are those that have an
increased risk of transmission, such as healthcare workers, incarcerated
people and patients on hemodialysis.”
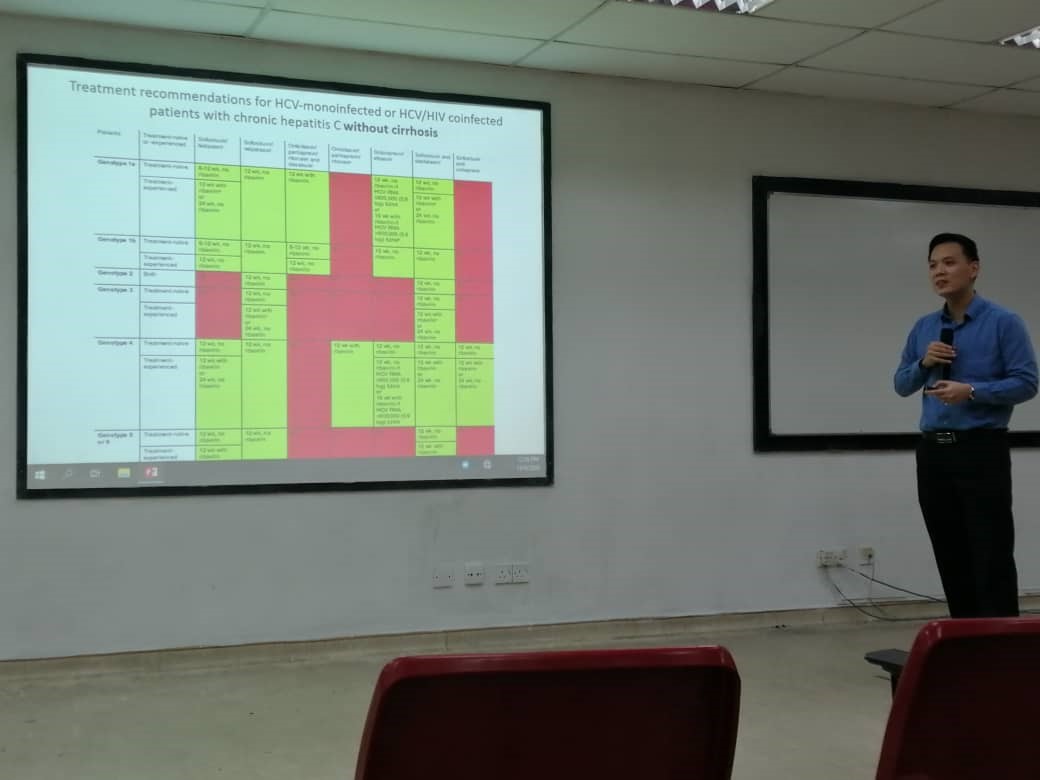
Dr Chung presenting
his slides
Dr Chung then described the HCV
pre-treatment assessment or the assessment of liver fibrosis in patients. He
pointed out several techniques to evaluate the prevalence of liver fibrosis;
“There is the normal liver ultrasound method and also the liver transient
elastography or also known as fibroscan, which is a non-invasive technique
that uses both ultrasound and low-frequency elastic waves to quantify liver
fibrosis. There is another method called the liver biopsy; this, however, is
less often used because it has a high mortality rate,” said Dr Chung.
Afterwards, he shared a roadmap of the progress that the medical world has
made, in terms of finding a cure for HCV. A noteworthy milestone that he
pointed out was during the 2000s, where Pegylated Interferon (PEG-IFN) and
Ribavirin were introduced, increasing the cure rate to almost 60 per cent.
Similarly, in 2011, the first antivirals, Boceprevir & Telaprevir were
combined with PEG-IFN and Ribavirin and it subsequently improved the cure
rate to 70 per cent. However, all these medications were ceased after a
while, due to the horrible side effects.
From there, he spoke on several other important topics, such as the HCV replication cycle and drug targets in Chronic Hepatitis C (CHC), the potential mechanism of action of Ribavirin in CHC treatment, Direct Acting Antivirals (DAAs) and Europe approved and recommended HCV DAAs. Dr Chung concluded the talk with a few key messages, whereby he mentioned that screening of high-risk individuals is very important and a cure is possible.

An enlightening Q&A session with Dr Chung

CRCD Chairperson Prof Dr Ngeow Yun Fong (right) presenting a token of appreciation to Dr Chung
![]()
Wholly owned by UTAR Education Foundation Co. No. 578227-M LEGAL STATEMENT TERM OF USAGE PRIVACY NOTICE