![]()
“Stroke is the second leading cause of death in the
Philippines. It has a prevalence of 0.9 per cent. Ischemic stroke comprises
70% while hemorrhagic stroke comprises 30%,” said Dr Peter Allan A.
Quitasol, a vascular neurologist and medical specialist II from the
Department of Neurology of Baguio General Hospital and Medical Center
Philippines at the webinar titled “The Sensing Brain: Stroke: Diagnosis and
Management”.
Held as part of the “Mind You Brain Series”, the
webinar was organised by UTAR Centre for Corporate and Community Development
in collaboration with Malaysia Mental Literacy Movement, Centre for Research
on Non-Communicable Diseases under UTAR M. Kandiah Faculty of Medicine and
Health Sciences (MK FMHS), and Faculty of Science on 9 November 2022 via
Zoom and Facebook Live.
Dr Peter Allan A. Quitasol
According to Dr Peter, stroke is a clinical syndrome
consisting of rapidly developing clinical signs of focal disturbance of
cerebral function secondary to a vascular event. “Stroke constitutes a major
contribution to morbidity and mortality in both developed and developing
countries,” said Dr Peter. He then explained the risk factors and the
subtypes of stroke, stroke recognition with BEFAST (Balance, Eyes, Face,
Arms, Speech and Time) and Neuroimaging.
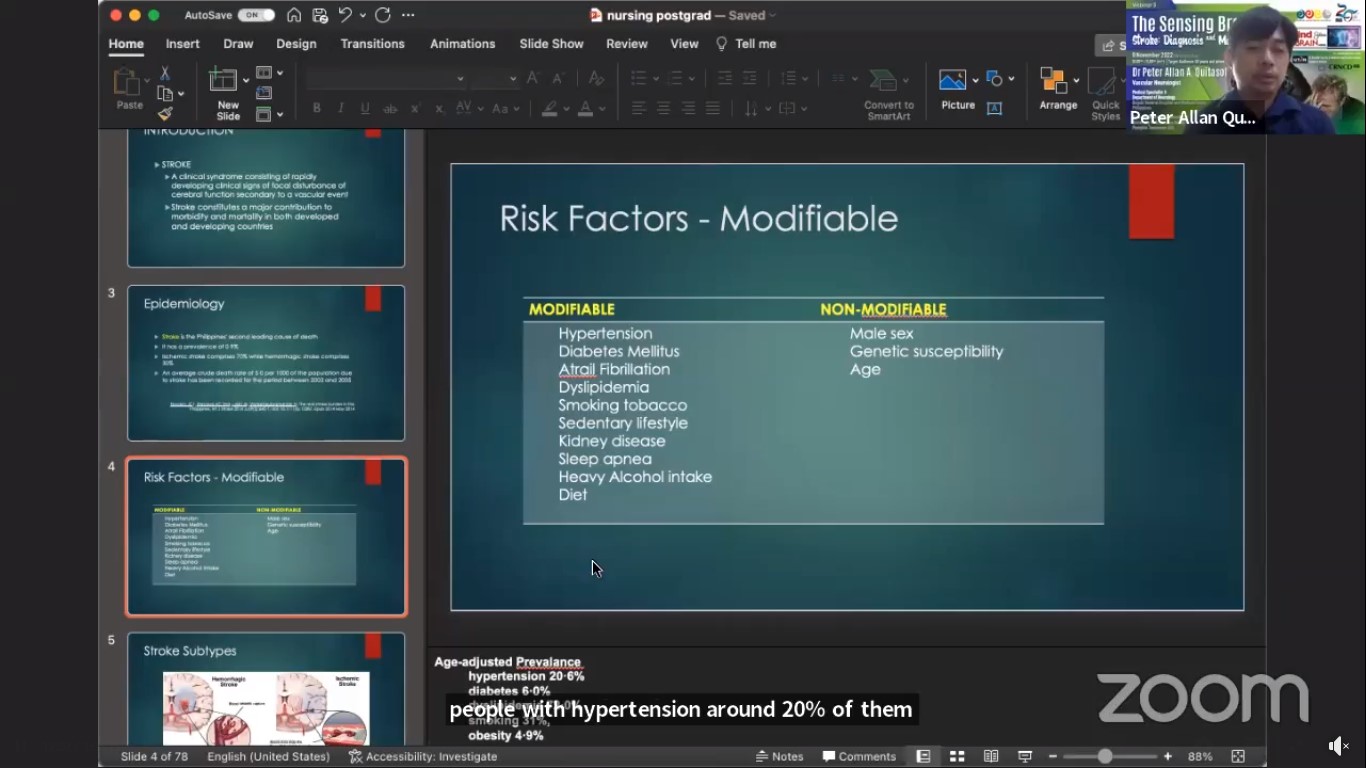
Risk factors of stroke
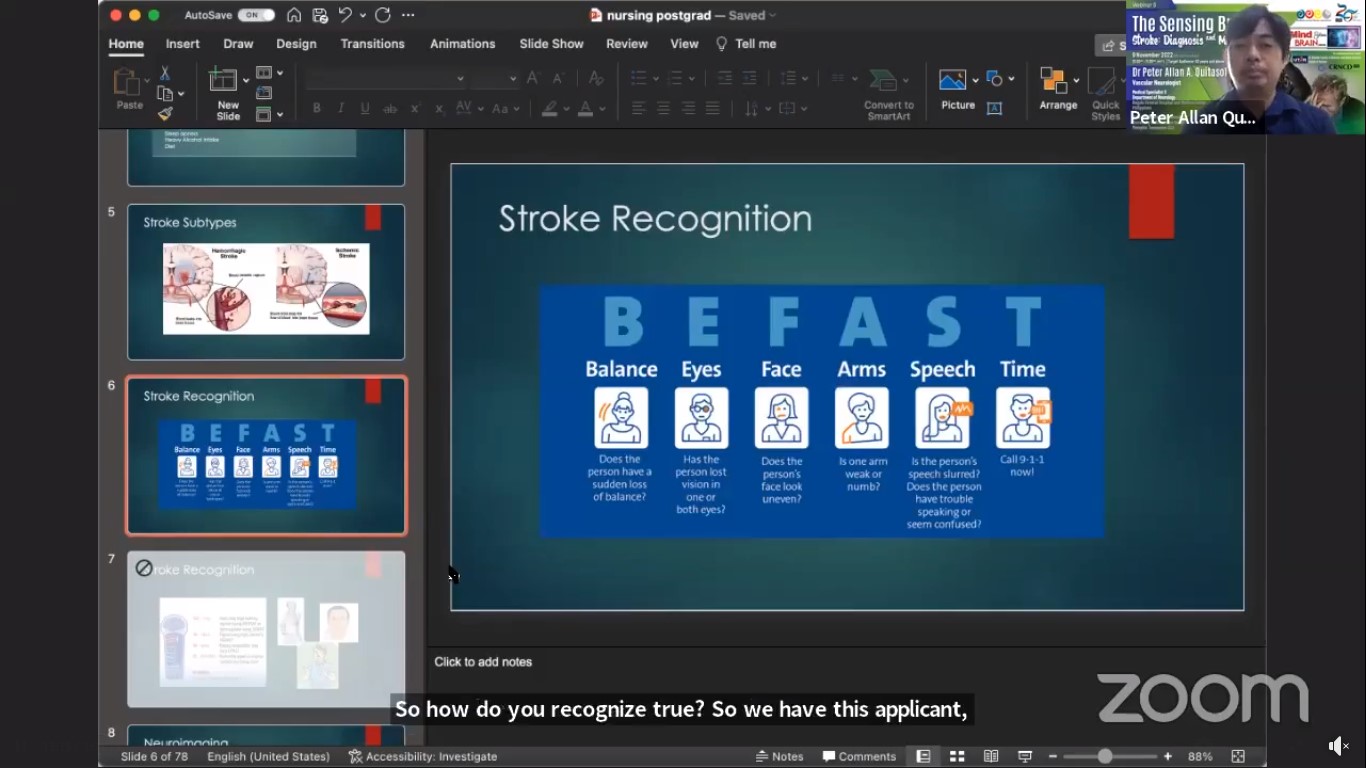
Stroke recognition with BEFAST
Besides explaining why stroke patients are rushed for
treatment, Dr Peter also shared the three main principles of acute stroke
care, which are to achieve timely recanalisation of the occluded artery and
reperfusion of the ischemic tissue, optimise collateral flow and avoid
secondary brain injury.
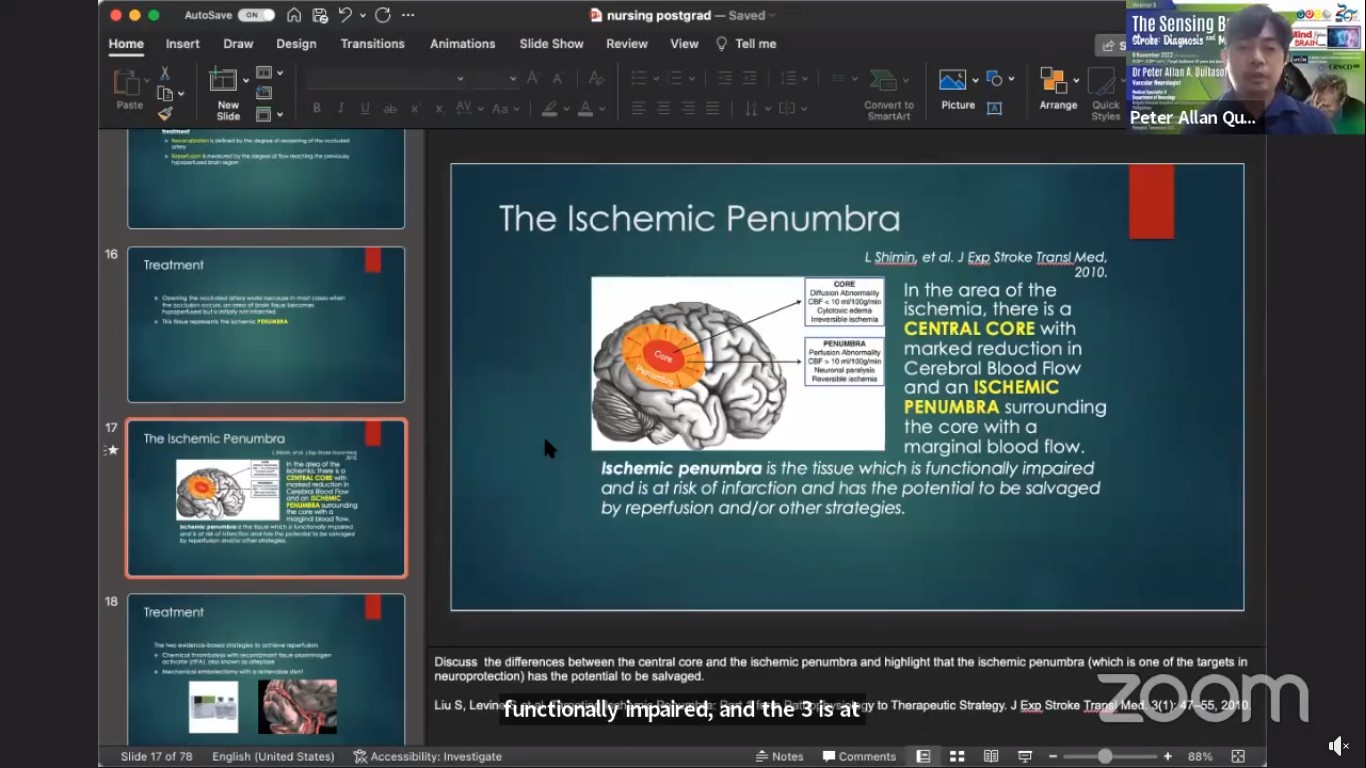
The ischemic penumbra
Speaking of Intravenous Thrombolysis, Dr Peter said,
“IV thrombolysis with rtPA is proven to be effective in improving functional
outcomes after an ischemic stroke up to 4.5 hours after symptom onset. IV
thrombolysis should not be withheld because of advanced age and mild but
disabling deficits.” He also shared about a useful tool for quantifying
neurologic impairment which is known as The National Institutes of Health
Stroke Scale, or NIH Stroke Scale (NIHSS). It enables the healthcare
provider to rapidly determine the severity and possible location of the
stroke.
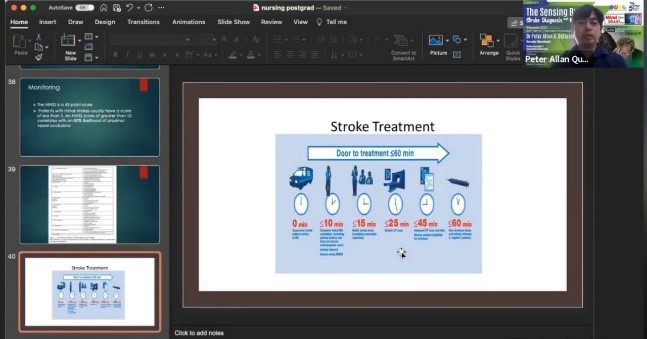
The timeline for stroke treatment
He said, “The human brain recovers from stroke
through adaptation, regeneration and neuroplasticity. Most stroke deficits
will see the highest rate of recovery during the first three to six months
after the stroke. We have a few types of therapy, namely physical therapy,
occupational therapy and speech therapy. Rehabilitation is a process of
stroke care that reduces disability and improves participation in therapy.
Recovery is defined as improvements across a variety of outcomes.”
He concluded, “Acute ischemic stroke is a medical
emergency in which every minute counts. Achievement of reperfusion can
reverse neurologic deficits, even if it is severe and allow patients to
regain function. There are two reperfusion strategies that are currently
proven. They are IV rtPA and mechanical thrombectomy. Patient selection is
crucial to optimise outcomes. The attitude of the clinician should be,
treatment must be given unless a solid contraindication exists. Stroke is a
‘brain attack’; it is an emergency but it is treatable and preventable.”
To watch the full webinar, kindly click
here.
Wholly owned by UTAR Education Foundation (200201010564(578227-M)) LEGAL STATEMENT TERM OF USAGE PRIVACY NOTICE